At the end of June 2000, Bill Clinton presented the design of the Human Genome Project to the White House. There, accompanied by scientists Francis Collins and Craig Venter and Tony Blair, the President of the United States announced the first results of a map that enabled us to decipher the Book of Life, our DNA. The sequencing of the genome made it possible to write a new chapter in the history of science.
Since then, reading thousands of genes from our species has enabled us to make progress in the fight against various diseases. A card, both in medicine and in real life, helps you know where to go. Thanks to the Human Genome Project, we now know better where we can look for some of the causes of major diseases and develop animal models to understand their development.
Almost two decades later, the scientific community has been working to create a new map, the so-called human cell atlas, to explore our body more closely. The aim is to map the number and type of cells that make up the body. “It is the next major project after genome sequencing and is likely to change the way cell and molecular biology is carried out in the future,” said Holger Heyn.
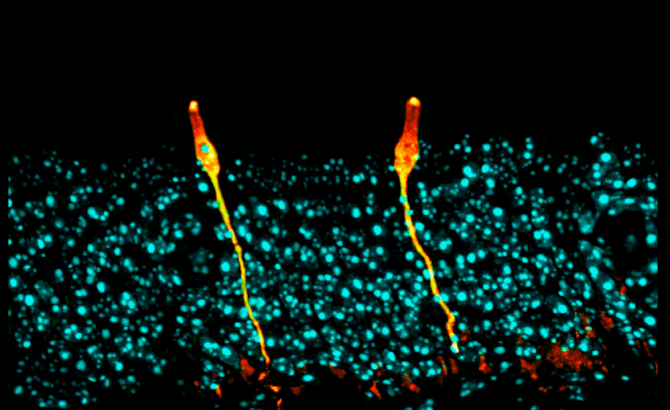
A team of researchers led by the Broad Institute at MIT and Massachusetts General Hospital (USA) has used state-of-the-art technologies to analyze cells at the individual level. Using methods for sequencing the RNA of each cell – the molecule produced from DNA to produce proteins – scientists have identified a new type of cell in mouse respiratory tissue and confirmed its results in human tissue. The results were published in the latest issue of Nature magazine.
After applying single-cell RNA sequencing to the respiratory tract of animal models, the researchers identified a rare cell type that represents less than 1% of the total population. The cells were called lung ionocytes because their pattern of gene expression is similar to that of ionocytes. These second specialized cells regulate the ion transport and hydration in the gills of fish and frog skin. In the case of lung ionocytes, scientists do not yet know what functions they can have, although they have discovered that they express several genes in connection with ion transport.
In particular, this apparently new cell type – which must be validated in further research – seems to play an important role in the regulation of a protein involved in cystic fibrosis. As they argue in nature, lung ionocytes would produce a molecule capable of controlling CFTR, a protein that facilitates the active transport of ions from the cells. Any failure of CFTR, as in cystic fibrosis patients, leads to an increase in the concentration of chlorine and sodium in the body secretion. In other words, very thick, sticky mucus builds up in such important organs as the lungs, pancreas, liver or intestines.
“Cystic fibrosis is an incredibly well-researched disease and we are still discovering a completely new biology that can change our approach,” said Jayaraj Rajagopal, a doctor at Massachusetts General Hospital, in a statement. The doctor emphasizes their surprise when they discovered that “most of the CFTR expression was in these rare cells”, a finding that they confirmed with a large amount of data from the Human Cell Atlas. The initiative was supported by the Chan Zuckerberg Initiative, which was driven by the creator of Facebook and contributed $15 million to the 85 research projects. The first raw data were published last April.